Appendicitis
What is appendicitis?
Appendicitis is a medical emergency. It happens when your appendix becomes sore, swollen, and diseased.
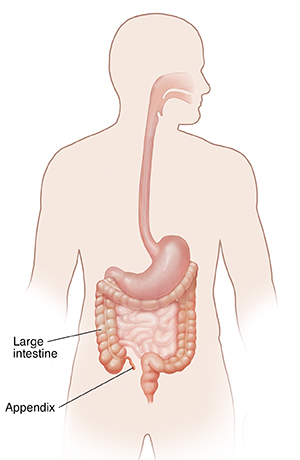
The appendix is a thin tube that is joined to the large intestine. It sits in the lower right part of your belly (abdomen). The appendix is a working part of your immune system. The immune system helps your body to fight disease.
The appendix can get infected and inflamed. If not treated, it can burst (rupture). This is serious and can lead to more infection and even death.
What causes appendicitis?
Appendicitis nearly always happens when the inside of your appendix gets blocked by something. This makes it swell up, and that makes the blockage worse. The bacteria that live in your intestines start an infection. If you have appendicitis, there is a serious risk that your appendix may burst. This can happen as soon as 48 to 72 hours after you start having symptoms. Because of this, appendicitis is a medical emergency. If you have symptoms, see your healthcare provider right away.
Appendicitis may be caused by various infections, such as viruses, bacteria, or parasites, in your digestive tract. Often, it may happen when the tube that joins your appendix with your large intestine gets blocked or trapped by stool. Sometimes tumors can cause appendicitis.
The appendix then becomes sore and swollen. The blood supply to the appendix stops as the swelling and soreness get worse. All of the organs in your body need the right amount of blood flow to stay healthy.
Without enough blood flow, the appendix starts to die. The appendix will burst as its walls start to get holes. These holes let stool, mucus, bacteria, and other things leak through and get inside your belly. You may get peritonitis. This is a serious infection throughout the belly that happens when the appendix or other part of the intestines or stomach has a hole and leaks out its contents.
Who is at risk for appendicitis?
Appendicitis is the most common cause of sudden (acute) belly pain that requires surgery. It mostly happens in teens and young adults in their 20s, but it can happen at any age. Having a family history of appendicitis may raise your risk, especially if you are a male.
What are the symptoms of appendicitis?
The following are common symptoms of appendicitis. Your own symptoms may vary.
Pain in the abdomen is the most common symptom. This pain:
-
May start around your belly button area and move to the lower right-hand side of your belly, or it may start in the lower right-hand side of your belly
-
Often gets worse as time goes on
-
May feel worse when you are moving, taking deep breaths, being touched, and coughing or sneezing
-
May be felt all over your belly if your appendix bursts
Other common symptoms include:
Do not take pain medicines. They may hide symptoms that your healthcare provider needs to know about.
Appendicitis symptoms may look like other health problems. Always see your healthcare provider to be sure.
How is appendicitis diagnosed?
Your healthcare provider will ask about your past health and do a physical exam. They may also order the following tests:
-
Blood tests. To check for signs of infection, such as having a high white blood cell count.
-
Urine tests. To see if you have a urinary tract infection.
You may also have some imaging tests, including:
-
Abdominal ultrasound (sonogram). This shows internal organs as they work and checks how blood is flowing through different blood vessels.
-
CT scan. This computerized X-ray shows detailed images of any part of the body, such as the bones, muscles, fat, and organs.
-
MRI. This scan uses a large magnet and radio waves to show different details than a CT scan. It is sometimes used to diagnose appendicitis, especially in a pregnant woman, instead of CT scan.
How is appendicitis treated?
Appendicitis is a medical emergency. It is likely the appendix will burst and cause a serious, deadly infection. For this reason, your healthcare provider will most likely tell you that you need to have surgery to remove your appendix.
The appendix will be removed in one of two ways:
-
Traditional (open) surgery method. You are given anesthesia. A cut (incision) is made in the lower right-hand side of your belly. The surgeon finds the appendix and takes it out. If the appendix has burst, a small drain may be put in to drain out pus and other fluids in the belly. The drain will be taken out in a few days, when your surgeon feels the infection has gone away.
-
Laparoscopic method. You are given anesthesia. This surgery uses several small cuts (incisions) and a camera (laparoscope) to look inside your belly. The surgical tools are placed through a few small cuts. The laparoscope is placed through another cut. A laparoscopy can often be done even if the appendix has burst.
If your appendix has not burst, your recovery from an appendectomy will take only a few days. If your appendix has burst, your recovery time will be longer, and you will need antibiotic medicine.
You will be treated for a few weeks with antibiotics and drainage if the infection around the appendix is too severe for immediate surgery. You will have surgery to remove the appendix at a later time.
Occasionally, appendicitis can be treated with antibiotics without surgery. However, these special cases are determined by your healthcare provider after an evaluation.
You can live a normal life without your appendix. Changes in diet or exercise are usually not needed.
What are possible complications of appendicitis?
The main problem with appendicitis is the risk of a burst appendix. This may happen if the appendix is not removed quickly. A burst appendix can lead to infection throughout the belly called peritonitis. Peritonitis can be very serious and even cause death if not treated right away.
Can appendicitis be prevented?
At this time, there is no known way to stop appendicitis from happening.
When should I call my healthcare provider?
If you have any of the symptoms of appendicitis listed above, call your healthcare provider right away. Or go to your closest emergency room. Appendicitis is a serious medical emergency. It should be treated as quickly as possible.
Key points about appendicitis
-
It is a medical emergency. You must seek care right away.
-
It happens when the inside of your appendix gets filled with something that causes it to swell, such as mucus, stool, or parasites.
-
Most cases of appendicitis happen between ages 10 and 30.
-
It nearly always causes pain in the belly, but each person may have different symptoms.
-
Your healthcare provider will tell you that you need to have surgery to remove your appendix.
-
You can live a normal life without your appendix.
Next steps
Tips to help you get the most from a visit to your health care provider:
-
Know the reason for your visit and what you want to happen.
-
Before your visit, write down questions you want answered.
-
Bring someone with you to help you ask questions and remember what your provider tells you.
-
At the visit, write down the name of a new diagnosis and any new medicines, treatments, or tests. Also write down any new instructions your provider gives you.
-
Know why a new medicine or treatment is prescribed and how it will help you. Also know what the side effects are.
-
Ask if your condition can be treated in other ways.
-
Know why a test or procedure is recommended and what the results could mean.
-
Know what to expect if you do not take the medicine or have the test or procedure.
-
If you have a follow-up appointment, write down the date, time, and purpose for that visit.
-
Know how you can contact your provider if you have questions.