Arrhythmias
What is an arrhythmia?
An arrhythmia is an abnormal heart rhythm.
Some arrhythmias can cause problems with contractions of your heart chambers by:
-
Not allowing the lower chambers (ventricles) to fill with enough blood, because an abnormal electrical signal is causing your heart to pump too fast or too slow.
-
Not allowing enough blood to be pumped out to your body, because an abnormal electrical signal is causing your heart to pump too slowly or irregularly.
-
Not allowing the top chambers (atria) to squeeze correctly.
An arrhythmia can occur in the sinus node, the atria, or the atrioventricular (AV) node. These are called supraventricular arrhythmias. Arrhythmias can also happen in your ventricles and are caused by an abnormal electrical focus. This results in abnormal conduction of electrical signals in your ventricles. Arrhythmias can also be listed as slow (bradyarrhythmia) or fast (tachyarrhythmia).
In any of these situations, your body's vital organs may not get enough blood to meet their needs.
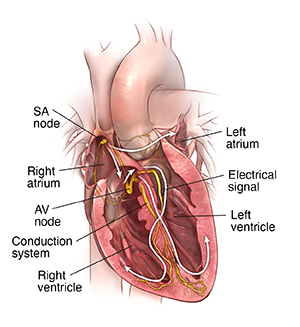 |
| Heart with normal conduction system. |
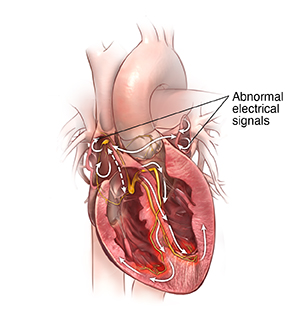 |
| Heart with arrhythmia. |
What causes an arrhythmia?
An arrhythmia happens when there is a problem with the electrical system that is supposed to control a steady heartbeat. With a problem in the electrical system, your heart may beat too fast, too slow, or irregularly.
Who is at risk for an arrhythmia?
Many things can affect the electrical system of your heart and cause an arrhythmia. Substances such as caffeine, alcohol, tobacco, illegal drugs, diet medicines, some herbs, and even prescription medicines can trigger an arrhythmia. Health conditions such as coronary heart disease, high blood pressure, sleep apnea, and diabetes raise your risk for arrhythmias. Arrhythmias become more common as you get older.
What are the symptoms of arrhythmias?
The effects on the body are often the same, whether the heartbeat is too fast, too slow, or too irregular. Some symptoms of arrhythmias include:
-
A fluttering feeling or irregular heartbeat (palpitations)
-
Weakness
-
Severe tiredness (fatigue)
-
Low blood pressure
-
Dizziness
-
Fainting
-
Heart failure
-
Collapse and cardiac arrest
-
Trouble feeding (in babies)
The symptoms of an arrhythmia may look like other conditions. Always see your healthcare provider for a diagnosis.
How are arrhythmias diagnosed?
Several tests may be used to diagnose arrhythmias.
Electrocardiogram (ECG). This test measures the electrical activity of your heart. Small sticky patches called electrodes are placed at specific locations on your body such as your chest, arms, and legs. The electrodes are connected to wires that pick up the heart's electrical activity and send it to the machine. The machine interprets the activity and makes a graph (tracing). An ECG can show:
-
An arrhythmia (both fast or slow ones)
-
Damage to the heart from a lack of oxygen to the heart muscle (ischemia) or a scar from a heart attack (also called a myocardial infarction)
-
Irregular interval measurements
-
Other types of heart condition
There are a few types of ECG tests:
-
Exercise ECG, or stress test. You are attached to the ECG machine as described above. But you walk on a treadmill or pedal a stationary bike while the ECG is recorded. This test is done to check for changes in the ECG during stress, such as exercise. If you're unable to exercise, the test may be done with your heart stressed by medicines.
-
Signal-averaged ECG. This procedure is done in the same way as a regular ECG. But this test records your heart's electrical activity for a longer time, often 15 to 20 minutes. Signal-averaged ECGs are done when your healthcare provider thinks you may have abnormal electrical conduction in the heart muscle. but it's not seen on a regular ECG. The signal-averaged ECG is more sensitive to problems in the ventricles called late potentials. Signal-averaged ECGs are used in research. In rare cases they may be used for routine evaluations.
-
Electrophysiologic studies (EPS). This is a nonsurgical but invasive test. A small, thin tube (catheter) is put into a large vein in your leg or neck and moved to your heart. This lets your provider test for arrhythmias and find where the arrhythmia starts within your heart tissue. Your provider can then figure out how to best treat it. Sometimes they can treat the arrhythmia by doing an ablation at the time of the study. An ablation creates scar tissue in the heart. This disrupts the abnormal electrical signal.
-
Holter monitor. A Holter monitor is a continuous ECG recording done over a period of 24 or more hours. Electrodes are attached to your chest and connected to a small portable ECG recorder by lead wires. Holter monitoring may be done when your provider thinks you may have an arrhythmia. Arrhythmias may last only a very short time. They may not be seen during the shorter recording time of a regular ECG. While wearing a Holter monitor, you can go about your daily activities. But you should not do things that cause a lot of sweating. This could cause the electrodes to become loose or fall off. You should also not take a shower or swim while wearing a Holter monitor. Newer Holter monitors don't require electrodes. Instead they are a single patch device attached to the skin over the heart.
-
Event monitor. This is a lot like a Holter monitor, except that you start the ECG recording only when you feel symptoms. Event monitors are typically worn longer than Holter monitors, for up to 30 days. You can remove the monitor to shower or bathe.
-
Mobile cardiac monitoring. This is a lot like Holter and event monitors. The ECG is constantly reviewed by a reading center to spot arrhythmias. The ECG is recorded and sent to your healthcare provider, whether or not you have symptoms. You can also start recordings yourself when you have symptoms. These monitors can be worn up to 30 days.
-
Implantable loop recorder. This is a miniature heart recording device that is implanted under the skin over your heart. It can record the heart rhythm for up to 3 to 4 years before the battery runs out. It's useful in diagnosing arrhythmias that happen only now and then or rarely.
How is an arrhythmia treated?
Some arrhythmias may cause few, if any, problems. In this case, you may not need treatment. When the arrhythmia causes symptoms, you have a few different choices for treatment. Your healthcare provider will discuss your treatment options with you. Together you will choose a treatment that is best for you. The choice will be based on the type of arrhythmia you have and how severe your symptoms are. It will also depend on if you have other conditions such as diabetes, kidney failure, or heart failure. These can affect the course of the treatment.
Some treatments for arrhythmias include:
-
Lifestyle changes. Stress, caffeine, and alcohol can cause arrhythmias. Your healthcare provider may advise you to not have caffeine, alcohol, or any other things that may be causing the problem. If your provider thinks that stress is a cause, they may suggest meditation, stress-management classes, an exercise program, or psychotherapy to ease stress.
-
Medicine. Medicine can treat arrhythmias. The medicine used will be based on the type of arrhythmia you have, if you have other health conditions, and if you take other medicines. Medicines may be used to slow down a fast arrhythmia or lower your chances for a stroke by keeping blood clots from forming.
-
Cardioversion. In this procedure, the healthcare provider sends an electrical shock to your heart through the chest. This may stop certain very fast arrhythmias such as atrial fibrillation, supraventricular tachycardia, or atrial flutter. You are connected to an ECG monitor, which is also connected to the defibrillator. The electrical shock is given at a point during the ECG cycle to change the rhythm to a normal one.
-
Ablation. This is an invasive but nonsurgical procedure done in the electrophysiology lab. The provider puts a thin, flexible tube (catheter) into your heart through a large vein in your groin or neck. The provider may use high-frequency radio waves to heat the tissue at the site of the arrhythmia and destroy it. This method is called radiofrequency ablation. Cryoablation is another method that can be used. For this, an ultra-cold substance is used to cool the tip of a catheter or balloon. This freezes and destroys the tissue.
-
Pacemaker. A permanent pacemaker is a small device that is put under the skin, often in the chest region just under the collarbone. It sends electrical signals to speed up a slow heartbeat. A permanent pacemaker may be used to make the heart beat if the heart's natural pacemaker (the SA node) is not working as it should, or if the electrical pathways are blocked. Pacemakers are often used for slow arrhythmias such as sinus bradycardia, sick sinus syndrome, or heart block.
-
Implantable cardioverter defibrillator (ICD). An ICD is a small device similar to a pacemaker. It's put under the skin, often just under the collarbone. An ICD senses the heart rhythm. When the device detects an abnormal rhythm, it sends an electrical shock to the heart. This corrects the rhythm to a more normal heart rhythm. Some ICDs can act as a pacemaker to send an electrical signal to adjust a slow heart rate. ICDs are often used for life-threatening fast arrhythmias such as ventricular tachycardia or ventricular fibrillation. A new generation of ICDs can now be placed in the left axillary region with a wire tunneled under the skin over the sternum. This ICD doesn't need a wire in the heart itself but can't act as a pacemaker.
-
Surgery. Surgery is usually done only when all other treatments have failed. Surgical ablation is major surgery that needs general anesthesia. The surgeon opens your chest or uses incisions in between the ribs to reach your heart. The surgeon destroys or removes the tissue causing the arrhythmia. This is most often used to treat advanced atrial fibrillation.
What are possible complications of an arrhythmia?
Some arrhythmias have no complications. But arrhythmias that are more serious can cause heart failure, stroke, or even cardiac arrest and death.
Living with an arrhythmia
Living with an arrhythmia includes making lifestyle changes such as not having caffeine, alcohol, or other triggers. It also includes taking medicines as directed. It may also include having a pacemaker or ICD inserted. If you have a pacemaker or ICD, ask your healthcare providers about any limits or lifestyle changes you may need to make. Working with your provider can promote your health and well-being.
When should I call my healthcare provider?
Tell your healthcare provider if:
-
Your symptoms get worse or you start to have new symptoms.
-
You have side effects from your medicine.
-
You need help with managing stress or emotions.
Key points about arrhythmias
An arrhythmia is an abnormal heart rhythm.
-
An arrhythmia can happen in the sinus node, the atria, or the atrioventricular node, or the ventricle.
-
Some arrhythmias cause few, if any, problems.
-
Other arrhythmias can cause serious complications such as heart failure, stroke, or even cardiac arrest and death.
-
Many treatment options are available to treat arrhythmia, including medicines, devices, cardiac ablation, and surgery. Many arrhythmias can be controlled with procedures.
Next steps
Tips to help you get the most from a visit to your healthcare provider:
-
Know the reason for your visit and what you want to happen.
-
Before your visit, write down questions you want answered.
-
Bring someone with you to help you ask questions and remember what your provider tells you.
-
At the visit, write down the name of a new diagnosis, and any new medicines, treatments, or tests. Also write down any new instructions your provider gives you.
-
Know why a new medicine or treatment is prescribed, and how it will help you. Also know what the side effects are.
-
Ask if your condition can be treated in other ways.
-
Know why a test or procedure is recommended and what the results could mean.
-
Know what to expect if you do not take the medicine or have the test or procedure.
-
If you have a follow-up appointment, write down the date, time, and purpose for that visit.
-
Know how you can contact your provider if you have questions.